Blank Ca Rfa PDF Form
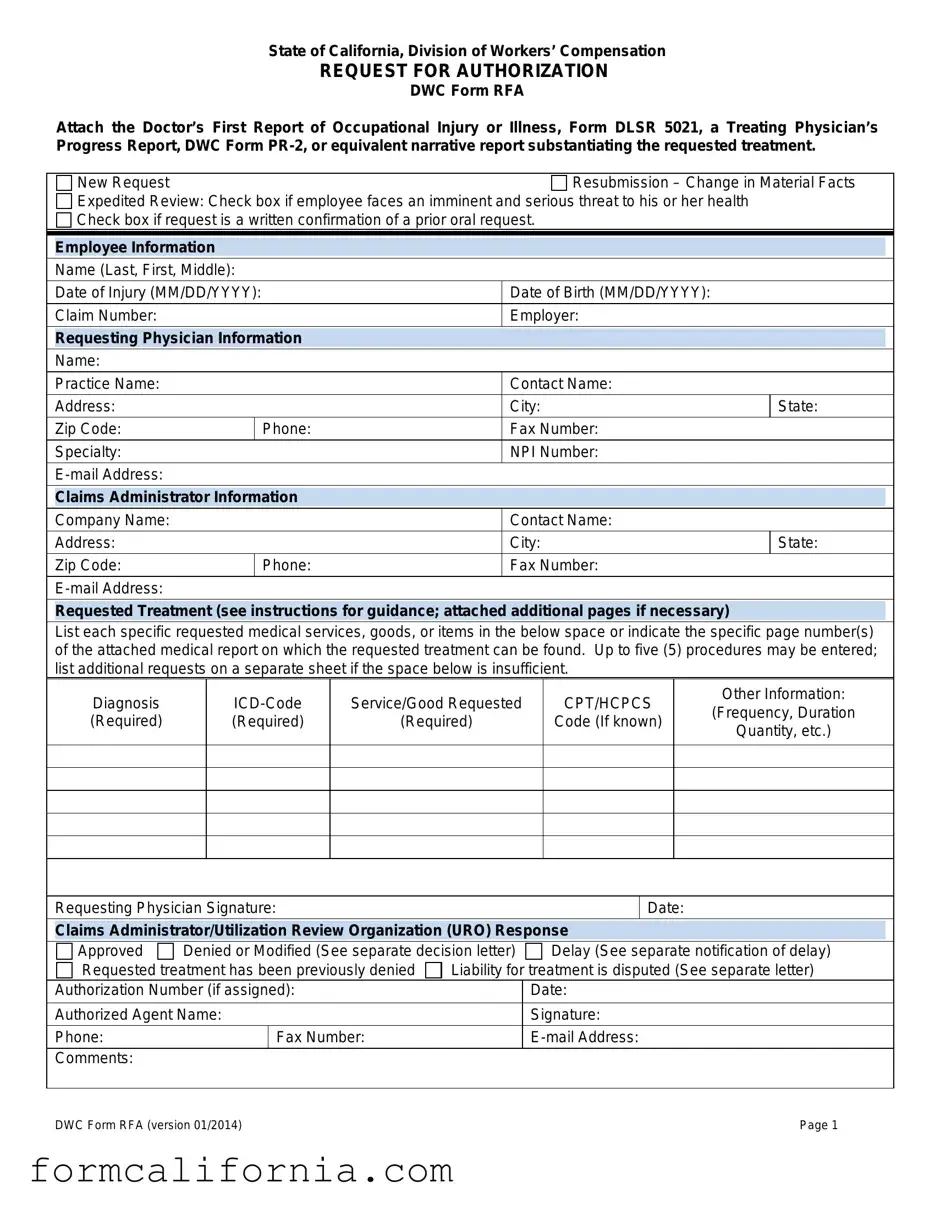
The State of California, through its Division of Workers' Compensation, has developed the Request for Authorization (RFA) form, known as DWC Form RFA, as a crucial document within the realm of workers' compensation medical care. This form plays an essential role in the utilization review process, which assesses the necessity and appropriateness of requested medical treatments for employees who have suffered occupational injuries or illnesses. To support a treatment request, the form mandates the attachment of substantiating reports such as the Doctor’s First Report of Occupational Injury or Illness, Form DLSR 5021, a Treating Physician’s Progress Report, DWC Form PR-2, or an equivalent narrative report. The form is designed to streamline the communication between the employee’s treating physician and the claims administrator or Utilization Review Organization, detailing new requests or resubmissions due to changed facts, and identifying whether an expedited review is necessary based on imminent health threats. Detailed information on the requested treatment, including diagnosis, treatment codes, and additional specifics such as frequency and duration, is required to thoroughly evaluate the necessity of the proposed medical service. The form ultimately facilitates a structured and efficient review process, ensuring timely and appropriate medical care for injured workers. It embodies a crucial step in managing workers' compensation claims, emphasizing the importance of clear, documented communication between medical providers and claims administrators for the benefit of employees in recovery.
Document Preview Example
State of California, Division of Workers’ Compensation
REQUEST FOR AUTHORIZATION
DWC Form RFA
Attach the Doctor’s First Report of Occupational Injury or Illness, Form DLSR 5021, a Treating Physician’s Progress Report, DWC Form
|
New Request |
|
Resubmission – Change in Material Facts |
|||
|
Expedited Review: Check box if employee faces an imminent and serious threat to his or her health |
|
|
|||
|
Check box if request is a written confirmation of a prior oral request. |
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Employee Information |
|
|
|
|
|
|
|
|
|
|
|
|
|
Name (Last, First, Middle): |
|
|
|
|
|
|
Date of Injury (MM/DD/YYYY): |
|
Date of Birth (MM/DD/YYYY): |
|
|
|
|
Claim Number: |
|
Employer: |
|
|
|
|
Requesting Physician Information |
|
|
|
||
|
|
|
|
|
|
|
|
Name: |
|
|
|
|
|
|
Practice Name: |
|
Contact Name: |
|
|
|
|
Address: |
|
City: |
State: |
||
|
Zip Code: |
|
Phone: |
Fax Number: |
|
|
|
Specialty: |
|
NPI Number: |
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
Claims Administrator Information |
|
|
|
||
|
|
|
|
|
|
|
|
Company Name: |
|
Contact Name: |
|
|
|
|
Address: |
|
City: |
State: |
||
|
Zip Code: |
|
Phone: |
Fax Number: |
|
|
Requested Treatment (see instructions for guidance; attached additional pages if necessary)
List each specific requested medical services, goods, or items in the below space or indicate the specific page number(s) of the attached medical report on which the requested treatment can be found. Up to five (5) procedures may be entered; list additional requests on a separate sheet if the space below is insufficient.
Diagnosis (Required)
Service/Good Requested
(Required)
CPT/HCPCS
Code (If known)
Other Information:
(Frequency, Duration
Quantity, etc.)
Requesting Physician Signature:
Date:
Claims Administrator/Utilization Review Organization (URO) Response
Approved |
Denied or Modified (See separate decision letter) |
Delay (See separate notification of delay) |
||
Requested treatment has been previously denied |
Liability for treatment is disputed (See separate letter) |
|||
Authorization Number (if assigned): |
|
Date: |
||
|
|
|
|
|
Authorized Agent Name: |
|
Signature: |
||
Phone: |
|
Fax Number: |
|
|
Comments: |
|
|
|
|
|
|
|
||
DWC Form RFA (version 01/2014) |
|
Page 1 |
||

Instructions for Request for Authorization Form
Warning: Private healthcare information is contained in the Request for Authorization for Medical Treatment, DWC Form RFA. The form can only go to other treating providers and to the claims administrator.
Overview: The Request for Authorization for Medical Treatment (DWC Form RFA) is required for the employee’s treating physician to initiate the utilization review process required by Labor Code section 4610. A Doctor’s First Report of Occupational Injury or Illness, Form DLSR 5021, a Treating Physician’s Progress Report, DWC Form
Checkboxes: Check the appropriate box at the top of the form. Indicate whether:
This is a new treatment request for the employee or the resubmission of a previously denied request based on a change in material facts regarding the employee’s condition. A resubmission is appropriate if the facts that provided the basis for the initial utilization review decision have subsequently changed such that the decision is no longer applicable to the employee’s current condition. Include documentation supporting your claim.
Review should be expedited based on an imminent and serious threat to the employee’s health. A request for expedited review must be supported by documentation substantiating the employee’s condition.
The request is a written confirmation of an earlier oral request.
Routing Information: This form can be mailed, faxed, or
Requested Treatment: The DWC Form RFA must contain all the information needed to substantiate the request for authorization. If the request is to continue a treatment plan or therapy, please attach documentation indicating progress, if applicable.
List the diagnosis (required), the ICD Code (required), the specific service/good requested (required), and applicable CPT/HCPCS code (if known).
Include, as necessary, the frequency, duration, quantity, etc. Reference to specific guidelines used to support treatment should also be included.
For requested treatment that is: (a) inconsistent with the Medical Treatment Utilization Schedule (MTUS) found at California Code of Regulations, title 8, section 9792.20, et seq.; or (b) for a condition or injury not addressed by the MTUS, you may include scientifically based evidence published in
Requesting Physician Signature: Signature/Date line is located under the requested treatment box. A signature by the treating physician is mandatory.
Claims Administrator/URO Response: Upon receipt of the DWC Form RFA, a claims administrator must respond within the timeframes and in the manner set forth in Labor Code section 4610 and California Code of Regulations, title 8, section 9792.9.1. To communicate its approval on requested treatment, the claims administrator may complete the lower portion of the DWC Form RFA and fax it back to the requesting provider. (Use of the DWC Form RFA is optional when communicating approvals of treatment; a claims administrator may utilize other means of written notification.) If multiple treatments are requested, indicate in comments section if any individual request is being denied or referred to utilization review.
DWC Form RFA (version 01/2014) |
Page 2 |
Document Specs
| Fact | Detail |
|---|---|
| Form Purpose | Initiate the utilization review process for medical treatment in workers' compensation cases. |
| Governing Law | Labor Code section 4610 and California Code of Regulations, title 8, section 9792.9.1. |
| Documentation Required | Doctor’s First Report of Occupational Injury or Illness, Form DLSR 5021, a Treating Physician’s Progress Report, DWC Form PR-2, or equivalent narrative report. |
| Report Reimbursement | Not reimbursable under the Official Medical Fee Schedule. |
| Expedited Review Criteria | Available if the employee faces an imminent and serious threat to his or her health. |
| Response Timeframe | A claims administrator must respond according to the timeframes set forth in Labor Code section 4610. |
| Medical Treatment Utilization Schedule (MTUS) Reference | For treatment inconsistent with MTUS or for a condition not addressed by MTUS, inclusion of scientifically based evidence is required. |
Detailed Instructions for Writing Ca Rfa
When submitting the Request for Authorization for Medical Treatment (DWC Form RFA) to initiate the utilization review process, it’s crucial to provide detailed and accurate information. This form, as mandated by Labor Code section 4610, plays a significant role in requesting medical treatment for employees. It ensures that the treating physician's request is considered under the utilization review to determine the necessity and appropriateness of proposed medical services. Completing and submitting this form accurately expedites the review process, aiding in timely decisions regarding the requested medical treatment.
- Begin with checking the appropriate box at the top of the form to indicate whether this is a New Request, a Resubmission – Change in Material Facts, or needs an Expedited Review due to an imminent and serious threat to the employee’s health. If the request confirms an earlier oral request, check the corresponding box.
- Fill in the Employee Information section with the employee's name (Last, First, Middle), date of injury (MM/DD/YYYY), date of birth (MM/DD/YYYY), claim number, and the employer's name.
- In the Requesting Physician Information section, provide the physician's name, practice name, contact name, their complete address including city, state, and zip code, phone and fax numbers, specialty, NPI number, and e-mail address.
- Complete the Claims Administrator Information section with the company name, contact name, address, city, state, zip code, as well as phone and fax numbers, and e-mail address.
- In the Requested Treatment section, list each requested medical service, good, or item. Include the diagnosis and ICD code (both required), as well as the service/good requested. If the CPT/HCPCS code is known, include it. Specify any necessary information like frequency, duration, and quantity.
- If the space provided is insufficient, attach additional pages as needed, clearly indicating the specific requests and any relevant information.
- Ensure that a Doctor’s First Report of Occupational Injury or Illness, Form DLSR 5021, a Treating Physician’s Progress Report, DWC Form PR-2, or an equivalent narrative report substantiating the requested treatment is attached.
- The Requesting Physician must sign and date the form under the requested treatment box to validate the request.
- Submit the completed form and any attachments to the claims administrator’s designated address, fax number, or e-mail address for processing.
Once submitted, the claims administrator must respond to the DWC Form RFA according to the statutes outlined in Labor Code section 4610 and the associated regulations. Their response—approving, denying, modifying, or delaying the requested treatment—will be communicated typically via fax, and it may include an authorization number or further instructions for the requesting physician. Timely submission and accurate completion of the DWC Form RFA facilitates the review process and supports the objective of providing necessary medical treatment to the employee.
Things to Know About This Form
What is the purpose of the DWC Form RFA?
The DWC Form RFA, or the Request for Authorization Form, is used in the state of California within the workers’ compensation system. Its primary purpose is to initiate the utilization review process for medical treatment requested by an employee's treating physician following a workplace injury or illness. The form serves as an official request to the claims administrator to authorize the proposed medical services, goods, or items. To support the request, it must be accompanied by documentation like the Doctor’s First Report of Occupational Injury or Illness, Form DLSR 5021, a Treating Physician’s Progress Report, DWC Form PR-2, or an equivalent narrative report that substantiates the need for the requested treatment.
How do I indicate the need for expedited review on the DWC Form RFA?
An expedited review of the DWC Form RFA can be requested if the employee is facing an imminent and serious threat to his or her health. To indicate the necessity of an expedited review, check the appropriate box at the top of the form. It's important to support the request with documentation substantiating the employee’s health condition that necessitates the urgent response. This ensures timely processing and review to address the critical health needs of the employee.
What information is required when completing the Requested Treatment section of the form?
The Requested Treatment section of the DWC Form RFA requires detailed information to effectively communicate the specific medical services, goods, or items being requested. Mandatory fields include:
- The diagnosis, with the required ICD Code.
- The specific service, good, or item requested, with the applicable CPT/HCPCS code if known.
- Additional details such as frequency, duration, and quantity.
If the treatment plan deviates from the Medical Treatment Utilization Schedule (MTUS), or addresses a condition not covered by it, justification based on peer-reviewed, nationally recognized scientific evidence must be included. Documentation of progress, if the request is for the continuation of a treatment plan, should also be attached.
What steps must be followed after completing the form?
Once the DWC Form RFA is completed and all necessary documentation is attached, it should be sent to the claims administrator's designated mailing address, fax number, or e-mail address. The treating physician must ensure that all required sections, including employee information, requesting physician information, and detailed requested treatment, are fully completed. The physician's signature at the end of the form is mandatory. After submission, the claims administrator will review the request and respond within the time frames established by Labor Code section 4610 and the California Code of Regulations. The response will indicate whether the treatment is approved, denied, modified, or delayed. A separate notification, such as a decision letter, will accompany any response other than full approval.
Common mistakes
When filling out the Request for Authorization (RFA) Form for workers' compensation in California, it's crucial to avoid common mistakes to ensure the timely and accurate processing of requests for medical treatment. Here are ten common errors to watch out for:
- Not attaching required medical reports: The RFA form requires attaching a Doctor's First Report of Occupational Injury or Illness, a Treating Physician’s Progress Report, or an equivalent narrative report. Failing to attach these documents can lead to delays.
- Incorrect or incomplete employee information: It's critical to accurately fill in the employee's name, date of injury, date of birth, and claim number. Incorrect information may result in processing delays or the denial of the request.
- Leaving physician information blank: The requesting physician's name, address, specialty, NPI number, and contact information must be fully and accurately provided to ensure proper communication.
- Incomplete claims administrator information: Accurate details of the claims administrator are necessary for appropriate routing and response to the RFA.
- Not specifying requested treatment: The form includes space to list specific medical services, goods, or items requested. Failure to specify these or attach additional pages if necessary can lead to incomplete understanding of the treatment needs.
- Omitting diagnosis and ICD code: Including the diagnosis and the corresponding ICD code is mandatory. Omitting this information will result in an incomplete request.
- Forgetting to include the service/good requested CPT/HCPCS code: While it might not always be known, providing the CPT/HCPCS code when available facilitates the timely review of the treatment request.
- Neglecting to detail frequency, duration, and quantity: When applicable, including details like how often and how long the treatment should last, as well as quantity, is essential for a complete treatment plan evaluation.
- Failure to sign the form: The treating physician's signature is mandatory on the RFA form. An unsigned form is considered incomplete and will not be processed.
- Not checking the appropriate box for expedited review or resubmission: For requests that require expedited review due to imminent and serious health threats or are resubmissions based on a change in material facts, the corresponding box at the top of the form must be checked. Lack of this indication may result in standard processing times being applied when expedited review is warranted.
Properly completing the RFA form by avoiding these common mistakes can significantly streamline the process of getting necessary medical treatment authorized for injured workers.
Documents used along the form
When navigating the complexities of workers' compensation in California, the Request for Authorization for Medical Treatment (DWC Form RFA) is a vital document that initiates the utilization review process for employees' medical treatment requests. However, to successfully undertake this process, various other forms and documents often accompany the DWC Form RFA, ensuring a comprehensive approach to managing and substantiating a worker's claim for medical benefits. Here's a closer look at some of these essential documents:
- Doctor's First Report of Occupational Injury or Illness (Form DLSR 5021): This is an initial report that a doctor completes when they first treat an employee for a work-related illness or injury. It provides crucial information about the nature and extent of the injury or illness.
- Treating Physician's Progress Report (DWC Form PR-2): Utilized as a follow-up to the initial report, this document details the employee's recovery progress, current condition, and any ongoing treatment needs. It's instrumental in substantiating the necessity for further medical authorization requested in the DWC Form RFA.
- Permanent and Stationary Report (P&S Report): Once an employee's condition stabilizes and is not expected to improve significantly, this report outlines the permanent impacts of the injury, including any lasting disabilities and the need for ongoing medical care or restrictions at work.
- Work Status Report: This document provides updates on the injured employee's ability to return to work, either in a limited, modified, or full capacity. It's crucial for determining the levels of work the employee can perform without aggravating their injury.
- Request for Supplemental Job Displacement Benefits (SJDB): If an employee cannot return to their former job due to the injury's limitations, they may be eligible for benefits under the SJDB. This form initiates the process to access training, education, or skill enhancement for alternative employment.
- Application for Adjudication of Claim: Should there be a dispute regarding the employee's workers' compensation benefits, this form officially brings the case in front of a Workers' Compensation Administrative Law Judge. It's necessary when resolution cannot be reached through standard claims review processes.
Together, these documents comprehensively support an employee's request for medical treatment following a work-related injury or illness. By accurately documenting every step from the injury's initial report to ongoing treatment and potential employment impact, these forms ensure that workers' compensation claims are thoroughly evaluated and justly administered. Understanding each document's role and requirement aids in navigating the complexities of workers' compensation claims, ensuring swift and fair resolution for both employees and employers.
Similar forms
The CA RFA form shares similarities with the Doctor's First Report of Occupational Injury or Illness, Form DLSR 5021. Both documents are integral parts of processing workers' compensation claims in California. The DLSR 5021 form serves as an initial report that a physician fills out upon the first examination of an injured worker, providing critical details about the injury and proposed treatment plan. Similarly, the RFA form is used by the treating physician to request authorization for specific medical treatments or services, making both forms pivotal in ensuring timely and appropriate medical care for injured workers.
Another document resembling the CA RFA form is the Treating Physician's Progress Report, DWC Form PR-2. This document, like the RFA, is used within the realm of workers' compensation to document the progress of a patient's treatment. The PR-2 often furnishes evidence supporting the need for continued or additional treatments, just as the RFA form requests authorization for specific interventions based on the patient’s current medical condition and treatment history.
The Utilization Review (UR) Request Form is also akin to the CA RFA form. Utilization Review is a process used by employers or their insurers to review the medical necessity of proposed treatments. Both forms play a role in this process; the RFA form is used to submit the treatment request, which is then reviewed according to UR standards. The main goal of both documents is to ensure that the proposed medical treatments are necessary and appropriate, reflecting their interconnected roles in managing healthcare within workers' compensation claims.
The Request for Second Opinion Form is somewhat similar to the CA RFA form, particularly in scenarios where there is a dispute or disagreement about the recommended treatment. While the RFA form is used to request authorization for specific treatments, the Request for Second Opinion Form allows injured workers to seek an additional medical opinion when they or the claims administrator have concerns about the recommended treatments. Both documents facilitate critical evaluations of proposed medical interventions, albeit from different perspectives.
The Medical Treatment Plan Template can be seen as analogous to the CA RFA form in its function to outline proposed medical treatments. While the RFA form is specifically used within the workers’ compensation system to seek authorization for such treatments, a Medical Treatment Plan Template is often used by healthcare providers to map out the course of treatment for various conditions. Both documents share the common goal of ensuring the patient receives appropriate and effective medical care.
The Request for Independent Medical Review (IMR) Form shares common ground with the CA RFA form, particularly in disputed workers' compensation cases. When a treatment authorization requested via an RFA form is denied or modified by the claims administrator, the injured worker can file an IMR form to dispute that decision. Thus, both forms are integral to the process of securing necessary medical treatment, though they serve different roles within the broader framework of dispute resolution.
The Prescription Drug Prior Authorization Request Form has parallels with the CA RFA form, as both involve the process of requesting approval before a specific treatment or medication is provided. In the context of workers' compensation, the RFA might include requests for prescription drugs as part of the treatment plan. The Prior Authorization Request Form serves a similar purpose in general healthcare, ensuring that prescribed medications are covered and deemed medically necessary before they are dispensed to the patient.
The Physical Therapy Request Form is another document similar to the CA RFA form since both may be used to request specific treatments within the scope of a patient’s recovery plan. In workers’ compensation cases, if physical therapy is deemed necessary for the injured worker’s rehabilitation, it would be requested through an RFA form. The Physical Therapy Request Form serves an analogous function outside the workers’ compensation system, requesting approval for physical therapy services to aid in a patient’s recovery.
Letter of Medical Necessity is related to the CA RFA form as they both are used to justify the need for specific medical treatments or services. A Letter of Medical Necessity is typically written by a healthcare provider to explain why a certain treatment or device is essential for the patient's condition, similar to how the RFA form substantiates the requested treatment with attached medical reports. Both documents are crucial in persuading insurance carriers or claims administrators of the importance and urgency of the proposed medical care.
Finally, the Workers' Compensation Claim Form (DWC-1) shares a connection with the CA RFA form, serving as the starting point in a workers' compensation case. While the DWC-1 form is used by the employee to initially report the injury or illness, the RFA form is a subsequent document used by the treating physician to request authorization for treatment. Both forms are critical steps in the process of securing medical care and benefits for injured workers, highlighting their role in navigating the workers' compensation system effectively.
Dos and Don'ts
Filling out the Request for Authorization (RFA) form accurately and completely is critical in the workers’ compensation process. To help ensure that your submission is processed efficiently and effectively, here are nine key guidelines:
- Do:
- Ensure all sections of the DWC Form RFA are filled out completely. Missing information can lead to unnecessary delays.
- Attach the required medical report to substantiate the requested treatment. This could be the Doctor’s First Report of Occupational Injury or Illness, Form DLSR 5021, a Treating Physician’s Progress Report, DWC Form PR-2, or an equivalent narrative report.
- Check the appropriate boxes at the top of the form to indicate whether it is a new request, a resubmission, or if an expedited review is needed.
- Include all relevant diagnosis and treatment information, such as the ICD Code and CPT/HCPCS Code (if known), and specifics about the requested treatment including frequency, duration, quantity, etc.
- Ensure the requesting physician signs and dates the form. This is a mandatory step for the form's acceptance.
- Don't:
- Forget to include any supporting documentation for expedited review requests or for treatments that are inconsistent with the Medical Treatment Utilization Schedule (MTUS).
- Leave out necessary routing information such as the contact details for the requesting physician and the claims administrator.
- Omit information about the diagnosis, requested treatment, and any specific page numbers of attached reports that justify the request.
- Use the form to communicate private health care information beyond the intended treating providers and claims administrator.
- Assume the form will be processed without the mandatory physician’s signature. Without it, the request is incomplete.
By following these guidelines, you can help streamline the utilization review process, ensuring timely and appropriate medical treatment for the injured worker. Remember, attention to detail can significantly impact the efficiency and outcome of your request.
Misconceptions
There are several common misconceptions about the California Request for Authorization Form (DWC Form RFA) that can lead to confusion for both healthcare providers and patients navigating the workers' compensation system. Understanding the facts can help in effectively managing treatment requests and ensuring that injured workers receive the necessary medical care.
- Misconception 1: Any medical report can be attached to the DWC Form RFA to substantiate the treatment request. In reality, the form requires specific documentation to substantiate the request for treatment. This includes a Doctor’s First Report of Occupational Injury or Illness (Form DLSR 5021), a Treating Physician’s Progress Report (DWC Form PR-2), or an equivalent narrative report highlighting the necessity of the requested treatment. Generic or irrelevant medical reports do not meet the documentation requirements.
- Misconception 2: The DWC Form RFA is itself a billable document under the Official Medical Fee Schedule. Contrary to this belief, the DWC Form RFA is not considered a separately reimbursable report under California's Official Medical Fee Schedule. It is crucial to understand that while the form initiates the utilization review process, it does not directly lead to payment for the provider.
- Misconception 3: Expedited reviews are granted for all urgent requests. While it is true that one can mark a request for expedited review in cases where the employee faces an imminent and serious health threat, such requests must be supported by adequate documentation. Merely checking the box for expedited review without providing the necessary substantiating evidence will not guarantee an accelerated consideration of the treatment request.
- Misconception 4: The response options on the DWC Form RFA are limited to "Approved" or "Denied". However, the response to a request for authorization by the claims administrator or Utilization Review Organization (URO) can be more nuanced, including options such as "Denied," "Modified," "Delay," or a declaration that liability for the treatment is disputed. It’s important for both requesting physicians and patients to be aware of all possible responses and understand that a denial or modification includes a separate detailed explanation or decision letter.
Correcting these misconceptions is crucial for managing expectations and ensuring a smoother process in the submission and response stages of treatment authorization under the California workers' compensation system.
Key takeaways
Understanding the Request for Authorization for Medical Treatment (DWC Form RFA) is vital for navigating workers' compensation medical requests in California effectively. Here are key takeaways to ensure the form is filled out and used correctly:
- Ensure all relevant sections of the DWC Form RFA are completed, including the attachment of a Doctor's First Report of Occupational Injury or Illness, a Treating Physician's Progress Report, or an equivalent narrative report to substantiate the requested treatment.
- Identify clearly whether the form is being submitted as a New Request or a Resubmission – Change in Material Facts, based on updated information regarding the employee’s condition that may affect the treatment approval.
- When an employee faces an imminent and serious threat to their health, mark the form for Expedited Review and provide necessary documentation to support this urgency.
- For written confirmations of verbal requests, ensure the appropriate box is checked to avoid processing delays.
- The physician must include detailed information on the requested treatment, including diagnosis, ICD Code, service or good requested, and, if known, the CPT/HCPCS code along with the frequency, duration, quantity, etc., as necessary.
- When treatments deviate from the Medical Treatment Utilization Schedule (MTUS), provide scientifically based evidence from peer-reviewed, nationally recognized journals to justify the request.
- The requesting physician’s signature is mandatory for the form’s validity, ensuring accountability and authenticity of the request.
- The form provides space to list up to five procedures. If more space is needed, attach additional sheets with the required information.
- Claims administrators must respond to the RFA within the timeframes specified in the Labor Code section 4610 and the California Code of Regulations, ensuring timely communication about the approval, denial, or modification of the requested treatment.
- The DWC Form RFA is not reimbursable under the Official Medical Fee Schedule, so it’s important not to anticipate additional payment for the completion and submission of this form.
The DWC Form RFA plays a crucial role in the workers' compensation process, ensuring employees receive timely and appropriate medical treatment for workplace injuries or illnesses. Diligently completing and using the form can streamline the utilization review process, fostering a smoother path to recovery for injured workers.
Discover More PDFs
Legal Guardianship California Form - GC-240 requires detailed information about the attorney or party acting without an attorney, including their state bar number and contact details.
Why Don't I Qualify for Dependent Care Credit - The inclusion of unearned income and other funds received offers a comprehensive approach to determining credit eligibility.