Blank Ca Participating Application PDF Form
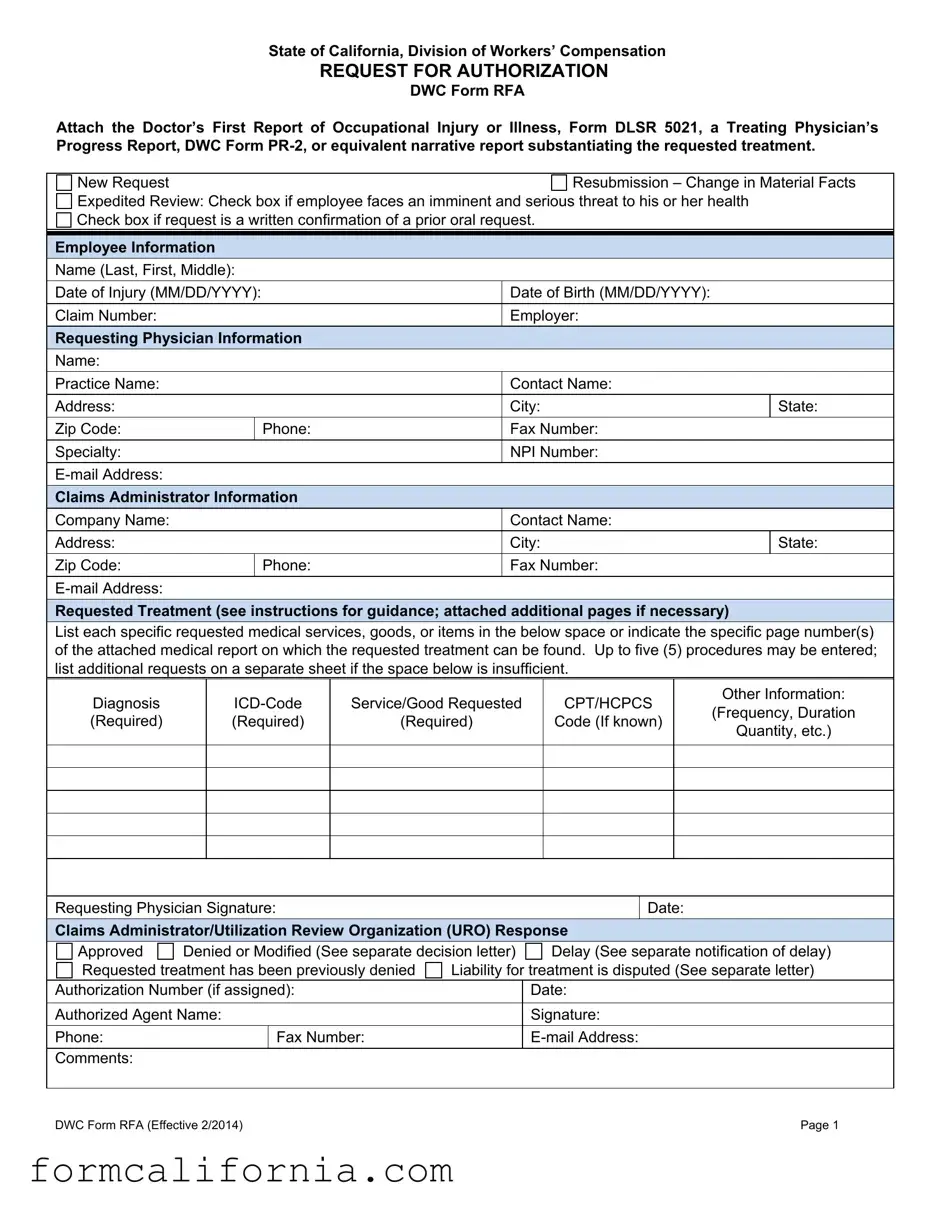
In the realm of workers' compensation within the State of California, the Division of Workers’ Compensation has established a structured protocol for requesting medical treatment through the Request for Authorization (DWC Form RFA). This mechanism is designed to streamline the process whereby an employee's treating physician can outline and substantiate the need for specific medical services, goods, or items following an occupational injury or illness. Critical to this form is the inclusion of supporting documentation, such as the Doctor’s First Report of Occupational Injury or Illness (Form DLSR 5021), a Treating Physician’s Progress Report (DWC Form PR-2), or an equivalent narrative report that details the medical rationales underpinning the treatment request. Further complexity is added by the provision for new requests, resubmissions upon a change in material facts about the employee's condition, and expedited reviews in cases where the employee's health faces immediate and weighty jeopardy. Additionally, the form necessitates comprehensive information about the employee, the requesting physician, and the claims administrator, ensuring all parties are correctly identified and informed. The DWC Form RFA not only facilitates the initial steps in the utilization review process, as mandated by Labor Code section 4610 but also, through its structured response section, lays the groundwork for the claims administrator's timely decision on the authorization, modification, or denial of the proposed medical treatment, emphasizing the procedural fidelity and accountability central to workers' compensation cases in California.
Document Preview Example
State of California, Division of Workers’ Compensation
REQUEST FOR AUTHORIZATION
DWC Form RFA
Attach the Doctor’s First Report of Occupational Injury or Illness, Form DLSR 5021, a Treating Physician’s Progress Report, DWC Form
New Request |
|
Resubmission – Change in Material Facts |
||
Expedited Review: Check box if employee faces an imminent and serious threat to his or her health |
|
|||
Check box if request is a written confirmation of a prior oral request. |
|
|||
|
|
|
|
|
Employee Information |
|
|
|
|
Name (Last, First, Middle): |
|
|
|
|
|
|
|
|
|
Date of Injury (MM/DD/YYYY): |
|
Date of Birth (MM/DD/YYYY): |
|
|
|
|
|
|
|
Claim Number: |
|
Employer: |
|
|
Requesting Physician Information |
|
|
||
Name: |
|
|
|
|
|
|
|
|
|
Practice Name: |
|
Contact Name: |
|
|
|
|
|
|
|
Address: |
|
City: |
State: |
|
|
|
|
|
|
Zip Code: |
|
Phone: |
Fax Number: |
|
|
|
|
|
|
Specialty: |
|
NPI Number: |
|
|
|
|
|
||
Claims Administrator Information |
|
|
||
Company Name: |
|
Contact Name: |
|
|
|
|
|
|
|
Address: |
|
City: |
State: |
|
|
|
|
|
|
Zip Code: |
|
Phone: |
Fax Number: |
|
|
|
|
|
|
|
|
|
||
Requested Treatment (see instructions for guidance; attached additional pages if necessary)
List each specific requested medical services, goods, or items in the below space or indicate the specific page number(s) of the attached medical report on which the requested treatment can be found. Up to five (5) procedures may be entered; list additional requests on a separate sheet if the space below is insufficient.
|
Diagnosis |
|
Service/Good Requested |
|
CPT/HCPCS |
|
Other Information: |
||||
|
|
|
|
(Frequency, Duration |
|||||||
|
(Required) |
|
(Required) |
(Required) |
|
Code (If known) |
|
||||
|
|
|
|
Quantity, etc.) |
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
Requesting Physician Signature: |
|
|
|
|
Date: |
|
||||
|
Claims Administrator/Utilization Review Organization (URO) Response |
|
|||||||||
|
Approved |
Denied or Modified (See separate decision letter) |
|
Delay (See separate notification of delay) |
|||||||
|
Requested treatment has been previously denied |
Liability for treatment is disputed (See separate letter) |
|||||||||
|
Authorization Number (if assigned): |
|
|
Date: |
|
||||||
|
|
|
|
|
|
|
|
||||
|
Authorized Agent Name: |
|
|
Signature: |
|
||||||
|
|
|
|
|
|
|
|
||||
|
Phone: |
|
|
Fax Number: |
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
Comments: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
DWC Form RFA (Effective 2/2014) |
|
|
|
|
|
|
Page 1 |
|||

Instructions for Request for Authorization Form
Warning: Private healthcare information is contained in the Request for Authorization for Medical Treatment, DWC Form RFA. The form can only go to other treating providers and to the claims administrator.
Overview: The Request for Authorization for Medical Treatment (DWC Form RFA) is required for the employee’s treating physician to initiate the utilization review process required by Labor Code section 4610. A Doctor’s First Report of Occupational Injury or Illness, Form DLSR 5021, a Treating Physician’s Progress Report, DWC Form
Checkboxes: Check the appropriate box at the top of the form. Indicate whether:
This is a new treatment request for the employee or the resubmission of a previously denied request based on a change in material facts regarding the employee’s condition. A resubmission is appropriate if the facts that provided the basis for the initial utilization review decision have subsequently changed such that the decision is no longer applicable to the employee’s current condition. Include documentation supporting your claim.
Review should be expedited based on an imminent and serious threat to the employee’s health. A request for expedited review must be supported by documentation substantiating the employee’s condition.
The request is a written confirmation of an earlier oral request.
Routing Information: This form can be mailed, faxed, or
Requested Treatment: The DWC Form RFA must contain all the information needed to substantiate the request for authorization. If the request is to continue a treatment plan or therapy, please attach documentation indicating progress, if applicable.
List the diagnosis (required), the ICD Code (required), the specific service/good requested (required), and applicable CPT/HCPCS code (if known).
Include, as necessary, the frequency, duration, quantity, etc. Reference to specific guidelines used to support treatment should also be included.
For requested treatment that is: (a) inconsistent with the Medical Treatment Utilization Schedule (MTUS) found at California Code of Regulations, title 8, section 9792.20, et seq.; or (b) for a condition or injury not addressed by the MTUS, you may include scientifically based evidence published in
Requesting Physician Signature: Signature/Date line is located under the requested treatment box. A signature by the treating physician is mandatory.
Claims Administrator/URO Response: Upon receipt of the DWC Form RFA, a claims administrator must respond within the timeframes and in the manner set forth in Labor Code section 4610 and California Code of Regulations, title 8, section 9792.9.1. To communicate its approval on requested treatment, the claims administrator may complete the lower portion of the DWC Form RFA and fax it back to the requesting provider. (Use of the DWC Form RFA is optional when communicating approvals of treatment; a claims administrator may utilize other means of written notification.) If multiple treatments are requested, indicate in comments section if any individual request is being denied or referred to utilization review.
DWC Form RFA (Effective 2/2014) |
Page 2 |
Document Specs
| Fact | Detail |
|---|---|
| Governing Law | Labor Code section 4610 and California Code of Regulations, title 8, section 9792.9.1. |
| Form Purpose | Initiate the utilization review process for requested medical treatment by the employee's treating physician. |
| Required Attachments | Doctor’s First Report of Occupational Injury or Illness, Form DLSR 5021, Treating Physician’s Progress Report, DWC Form PR-2, or equivalent narrative report. |
| Form Sections | New Request, Resubmission – Change in Material Facts, Expedited Review. |
| Routing Information | Can be mailed, faxed, or emailed to the claims administrator. |
| Requested Treatment Details | Lists diagnosis, ICD Code, specific service/good requested, CPT/HCPCS code, frequency, duration, quantity, etc. |
| Mandatory Signature | Requesting physician's signature is mandatory for form submission. |
| Claims Administrator/URO Response | Must respond within defined timeframes and manner as per Labor Code section 4610 and California Code of Regulations, title 8, section 9792.9.1. |
Detailed Instructions for Writing Ca Participating Application
Filling out the Request for Authorization for Medical Treatment (DWC Form RFA) is a critical step in ensuring that employees receive the proper workers' compensation benefits for healthcare treatments. This form kicks off the utilization review process, which determines whether the requested medical treatment for an occupational injury or illness is authorized under California's workers' compensation laws. Accurate and thorough completion of this form is essential to facilitate a smooth review process and to help ensure that workers receive the necessary medical care without undue delay.
- Start by checking the appropriate box at the top of the form to indicate whether this is a New Request, a Resubmission – Change in Material Facts, or if an Expedited Review is necessary due to an imminent and serious threat to health. Check another box if the request is confirming a prior oral request.
- Complete the Employee Information section with the employee's name, date of injury, date of birth, claim number, and employer.
- In the Requesting Physician Information section, enter the physician's name, practice name, contact name, full address, phone and fax numbers, specialty, NPI number, and email address.
- Fill out the Claims Administrator Information section with the company name, contact name, address, city, state, zip code, phone and fax numbers, and email address.
- For the Requested Treatment section, list each specific medical service, good, or item being requested. Include the diagnosis, ICD code, service/good requested, applicable CPT/HCPCS code if known, and other relevant information such as frequency, duration, and quantity. Attach additional pages if necessary and reference any specific guidelines or peer-reviewed evidence supporting the treatment.
- Ensure that required attachments, such as a Doctor’s First Report of Occupational Injury or Illness (Form DLSR 5021), a Treating Physician’s Progress Report (DWC Form PR-2), or an equivalent narrative report substantiating the requested treatment, are securely attached to the DWC Form RFA.
- Sign and date the form under the Requesting Physician Signature section to verify the accuracy and completeness of the request.
- Review the form for completeness and accuracy before sending it to the claims administrator via mail, fax, or email, using the routing information provided by the claims administrator.
Upon submission, the claims administrator will review the DWC Form RFA and respond within the timeframes specified by labor laws. The response will be communicated through a decision letter stating whether the requested treatment is approved, denied, modified, delayed, or if liability for treatment is disputed. Understanding the claims administrator’s feedback and following up as necessary is key to managing the employee's treatment plan and ensuring they receive appropriate care.
Things to Know About This Form
What is the purpose of the DWC Form RFA?
The DWC Form RFA, or Request for Authorization for Medical Treatment, is a crucial document used in the workers' compensation system in California. Its primary purpose is to initiate the utilization review process as required by Labor Code section 4610. This process assesses the necessity and appropriateness of requested medical treatment for employees who have suffered a work-related injury or illness. To substantiate the request for treatment, the form must be accompanied by relevant medical reports, such as a Doctor’s First Report of Occupational Injury or Illness (Form DLSR 5021), a Treating Physician’s Progress Report (DWC Form PR-2), or an equivalent narrative report.
What documentation must accompany the DWC Form RFA?
To ensure a comprehensive evaluation, the DWC Form RFA must be submitted with supporting documentation. This includes one of the following: a Doctor’s First Report of Occupational Injury or Illness, Form DLSR 5021; a Treating Physician’s Progress Report, DWC Form PR-2; or an equivalent narrative report that substantiates the requested treatment. These documents provide detailed information about the injury or illness and the rationale behind the requested treatment or therapy.
What are the checkboxes at the top of the DWC Form RFA for?
The checkboxes at the top of the DWC Form RFA are designed to indicate the type of request being made. There are three main options:
- A new treatment request for the employee.
- A resubmission of a previously denied request, based on a change in material facts regarding the employee's condition.
- A request for expedited review if the employee faces an imminent and serious threat to their health. This must be supported with documentation.
How is the DWC Form RFA submitted?
The DWC Form RFA can be submitted through various methods, depending on the preferences of the claims administrator. It can be mailed, faxed, or emailed to the designated address, fax number, or email address provided by the claims administrator. It's important that the requesting physician completes all sections of the form, including detailed information about the employee, the claims administrator, and the physician.
What information is required on the DWC Form RFA?
The form requires comprehensive information to substantiate the request for medical treatment, including:
- The diagnosis with the required ICD Code.
- The specific services, goods, or items requested, including applicable CPT/HCPCS codes, if known.
- Details such as frequency, duration, and quantity of the requested treatment.
Is the requesting physician's signature required on the DWC Form RFA?
Yes, the requesting physician must sign and date the DWC Form RFA. This confirms that the physician has reviewed the request and believes that the proposed treatment is necessary for the employee's work-related injury or illness. The signature is located under the requested treatment section of the form.
How does the claims administrator respond to the DWC Form RFA?
Upon receipt of the DWC Form RFA, the claims administrator has specific timeframes and procedures to follow as outlined in Labor Code section 4610 and California Code of Regulations, title 8, section 9792.9.1. The administrator must provide a response indicating approval, denial, or modification of the requested treatment. This can be communicated through faxing the completed lower portion of the DWC Form RFA back to the requesting provider or through other written notifications.
What happens if multiple treatments are requested?
If the DWC Form RFA includes requests for multiple treatments, the claims administrator must clearly indicate in the comments section of the form which requests, if any, are being denied or referred to utilization review. It allows for a detailed and organized response to each specific treatment request made on behalf of the employee.
Is the DWC Form RFA reimbursable under the Official Medical Fee Schedule?
No, the DWC Form RFA is not considered a separately reimbursable report under the Official Medical Fee Schedule, as found in the California Code of Regulations, title 8, section 9789.10 et seq. It is a required form designed to facilitate the utilization review process but does not qualify for reimbursement in itself.
Common mistakes
Filling out the Request for Authorization (RFA) form accurately is essential for obtaining timely approval for workers' compensation medical treatments in California. Yet, there are common oversights people make during this process. Recognizing and avoiding these mistakes can streamline the approval process, ensuring that employees receive the care they need without unnecessary delays.
Not attaching the required reports: A crucial mistake is failing to attach a Doctor's First Report of Occupational Injury or Illness, Form DLSR 5021, a Treating Physician’s Progress Report, DWC Form PR-2, or an equivalent narrative report that substantiates the requested treatment. This documentation is essential for initiating the utilization review process.
Incorrect or incomplete employee information: The RFA form requires specific details about the employee, including their name, date of injury, date of birth, and claim number. Omitting any of these details or providing inaccurate information can lead to delays in the review process.
Oversights in the requesting physician section: The form asks for comprehensive information about the requesting physician, including their name, practice name, contact details, and National Provider Identifier (NPI) number. Sometimes, people forget to fill out some of these fields or enter incorrect information, impeding communication and processing.
Failing to check the correct boxes: At the top of the form, it's important to indicate whether the request is new, a resubmission due to a change in material facts, or if an expedited review is required due to a serious threat to the employee’s health. Missing or incorrectly marking these boxes can divert the application to the wrong process.
Inadequate description of requested treatment: The RFA form mandates a detailed listing of the requested medical services, goods, or items, including diagnosis, ICD codes, and the specific service/good requested. Neglecting to provide detailed information or not attaching additional pages if the space below is insufficient can lead to a denial or delay in authorization.
Forgetting the requesting physician’s signature: A common yet critical error is not having the treating physician sign the form. The signature and date line located under the requested treatment box must be completed to validate the request. This oversight can invalidate the whole application process.
By paying attention to these details, the accuracy and completeness of the RFA submission can be ensured, facilitating a smoother approval process for the necessary medical treatment.
Documents used along the form
In the framework of workers' compensation in the state of California, the Request for Authorization for Medical Treatment (DWC Form RFA) plays a pivotal role. This form initiates the utilization review process, ensuring that employees receive necessary medical care. However, this form does not function in isolation. There are several other forms and documents that often accompany the DWC Form RFA, each serving a distinct purpose in the broader context of workers' compensation claims management and compliance.
- Doctor’s First Report of Occupational Injury or Illness (Form DLSR 5021): This form provides initial information regarding an occupational injury or illness. It is a mandatory report that must be completed by the physician who first treats the employee for the work-related injury or illness. The form documents the nature of the injury or illness, the initial treatment provided, and the prognosis.
- Treating Physician’s Progress Report (DWC Form PR-2): This form is used by the treating physician to report the progress of the employee after the initial treatment. It includes information about the employee's current medical status, details of any ongoing treatment, any changes in the diagnosis or prognosis, and plans for future medical care. This form is crucial for evaluating the necessity and efficacy of the ongoing treatment.
- Employee Claim Form (DWC Form 1): After sustaining a work-related injury or illness, an employee uses this form to formally report the incident and file a claim for workers' compensation benefits. It captures essential information about the employee, the employer, the circumstances of the injury or illness, and the types of benefits being sought.
- Utilization Review (UR) Decision Letter: This is not a form but a letter generated by the claims administrator after reviewing the Request for Authorization (RFA) under the UR process. It details the decision regarding the requested medical treatment — whether it's approved, modified, or denied. The letter includes reasons for the decision, instructions for appealing the decision if necessary, and often references medical guidelines or evidence considered in the decision-making process.
- Application for Adjudication of Claim (DWC Form ADJ): If there is a dispute regarding the workers' compensation claim, including issues related to the authorization of medical treatment, this form is used to file a case with the Workers' Compensation Appeals Board (WCAB). It provides a formal avenue for resolving disputes between the employee and the employer (or insurance carrier).
Together, these documents ensure a structured approach to managing and administering workers' compensation claims in California. They facilitate the process from the initial reporting of an injury, through the medical treatment authorization process, to resolving disputes when necessary. Each document has a defined role, contributing to a system designed to protect injured workers while ensuring that the treatment they receive is appropriate, necessary, and in accordance with established guidelines.
Similar forms
The Ca Participating Application form, specifically the Request for Authorization (RFA) for DWC, shares similarities with several other medical and legal documents, each serving unique yet interconnected roles within the landscape of workers' compensation and healthcare administration. By examining these documents, one can appreciate the nuances and specificities that define and distinguish each within their respective domains.
Firstly, the Doctor’s First Report of Occupational Injury or Illness, Form DLSR 5021, parallels the RFA in its foundational role within workers' compensation claims. This form initiates the claim by documenting the initial injury or illness, similar to how an RFA requests specific medical treatment based on the condition outlined in the DLSR 5021. Both are critical early steps in processing a worker’s compensation case, with one identifying the problem and the other proposing a solution.
The Treating Physician’s Progress Report, DWC Form PR-2, serves a continuation of the narrative that begins with the RFA. Where the RFA might request specific treatments, the PR-2 documents the outcome of those treatments over time. It’s a dialogue between the initial request and the ongoing response, showcasing how treatments are affecting the patient's recovery process.
An equivalent narrative report, while not a standardized form like the RFA, complements it by providing detailed medical explanations and rationales for the requested treatments. These narrative reports offer depth and context, helping claims administrators and review organizations understand the necessity and appropriateness of the treatments sought.
The Request for Summary Rating Determination of Qualified Medical Evaluator (QME) Form, while serving a different function, relates to the RFA by being another step in the broader process of resolving a workers' compensation claim. While the RFA deals with immediate treatment needs, the QME form plays a pivotal role in the determination of permanent disability and potential settlement amounts.
Utilization Review (UR) forms, though varied, have a direct relationship with the RFA. The RFA is subject to review by the UR process, which evaluates the necessity and effectiveness of proposed treatments. This ensures that the treatments are in line with medical guidelines and are likely to benefit the patient, making these forms administrative counterparts.
Application for Adjudication of Claim, another document within the workers' compensation realm, though focusing on disputes over claims, intersects with the RFA process. An RFA may lead to this form if there is disagreement between the employee and employer (or insurer) about the authorization of the requested medical treatment.
The Declaration of Readiness to Proceed form, used when a party is ready to move forward to a hearing regarding a workers' compensation claim, might come into play if issues around the RFA, such as denial of treatment, cannot be resolved through negotiation or mediation. It signifies escalation in the dispute resolution process, indirectly linked to the outcomes of RFA submissions.
Finally, the Compromise and Release form, a legal document used to settle a workers' compensation claim, can sometimes be the endpoint of a journey that begins with an RFS. If treatments requested through RFAs lead to a satisfactory recovery, a Compromise and Release may be executed to resolve the claim entirely. It represents a closure that often starts with the medical treatment authorization sought through an RFA.
Each of these documents, though serving distinct purposes, plays a role in the intricate process of managing, adjudicating, and resolving workers' compensation claims. Together, they form a comprehensive system that addresses the needs of injured workers, from initial injury reporting to treatment authorization and, ultimately, to claim resolution.
Dos and Don'ts
Filling out the CA Participating Application form accurately is crucial for the timely processing of workers' compensation medical requests. Below are five things you should do and five things you shouldn't do when completing this form.
What You Should Do:
Always attach the requisite medical reports — either the Doctor’s First Report of Occupational Injury or Illness, the Treating Physician's Progress Report, or an equivalent narrative report that substantiates the treatment request.
Check the correct box at the top of the form to indicate whether this is a new request, a resubmission due to a change in material facts, or if an expedited review is needed because the employee faces an imminent and serious threat to their health.
Provide complete and accurate information for the employee, the requesting physician, and the claims administrator, including all required contact information.
List each specific requested medical service, good, or item clearly, including the required diagnosis and ICD Code, and, if known, the applicable CPT/HCPCS code. If the space provided is insufficient, attach additional pages as necessary.
Ensure that the requesting physician signs and dates the form. The signature is mandatory for the form to be processed.
What You Shouldn't Do:
Don't leave out any required information, such as the diagnosis ICD Code or the specific service or good requested. Incomplete forms can cause delays.
Avoid submitting the form without the required attachments that justify the requested treatment, as this will likely result in a denial or delay.
Don't forget to check the box for an expedited review if the employee’s condition warrants it, but also be sure this request is substantiated with the appropriate documentation.
Never submit the form without a signature from the requesting physician. An unsigned form is considered incomplete.
Avoid using outdated contact information for either the requesting physician or the claims administrator to prevent delays in communication.
Misconceptions
When it comes to navigating the complexities of the California Participating Application form, or the DWC Form RFA, there are several misconceptions that can lead to confusion for both providers and patients. Understanding the truth behind these common misunderstandings can help streamline the process of requesting authorization for medical treatment under workers’ compensation.
It's only for initial treatment requests: Many believe the DWC Form RFA is solely for initiating treatment. However, the form is also crucial for resubmitting previously denied requests if there’s a change in material facts or for requesting expedited review due to serious and imminent health threats.
Email isn't an option for submission: Contrary to what some think, this form can be submitted through various channels, including mail, fax, and email, as long as it's directed to the designated claims administrator contact details.
Any medical documentation will suffice: The form requires specific attachments, like the Doctor’s First Report of Occupational Injury or Illness, Form DLSR 5021, or a progress report; not just any medical document can accompany this form.
The form is separately billable: Some might assume that submitting this form could be separately reimbursable under the Official Medical Fee Schedule. In reality, it is not a billable document.
No need for detailed treatment information: The form necessitates detailed information about the requested treatment, including diagnosis, ICD Code, and CPT/HCPCS codes, if available. It’s not sufficient to simply state the treatment without specific details.
All treatments get approved through this form: The submission of a DWC Form RFA does not guarantee approval. The request undergoes a utilization review process, and treatments can be approved, denied, or modified based on this review.
One form per treatment: A common misbelief is that each treatment request needs its own form. In reality, up to five procedures can be listed on one form, with additional requests on separate sheets if needed.
Physician’s signature isn’t mandatory: Actually, the requesting physician’s signature is a crucial component of the form. This authenticates the request and is a mandatory requirement for processing.
Immediate approval for expedited cases: Although the form has a provision for expedited review in urgent cases, it still requires documentation to substantiate the health threat, and approval is not instantaneous.
Utilization review outcomes are final: The responses from the claims administrator or Utilization Review Organization can lead to disputes. Denied or modified treatments can be contested through further documentation or appeals, indicating the outcome is not always final on first review.
By demystifying these misconceptions, both healthcare providers and patients can better navigate the process of securing necessary treatments through the DWC Form RFA, leading to a smoother and more efficient workers’ compensation claims process.
Key takeaways
Understanding the DWC Form RFA is crucial for initiating the utilization review process in workers’ compensation cases in California.
When employees seek medical treatment for a work-related injury or illness, their treating physicians must complete the Request for Authorization for Medical Treatment (DWC Form RFA). This form triggers the formal review process required by the state to assess and approve necessary medical care. Here are five key takeaways for effectively filling out and using this form:
- Required Attachments: Completing the DWC Form RFA requires attaching a Doctor’s First Report of Occupational Injury or Illness, a Treating Physician’s Progress Report, or an equivalent narrative report that substantiates the need for the requested treatment. This documentation is essential to justify the medical services, goods, or items requested.
- Expedited Review Option: If the employee’s health is in imminent and serious jeopardy, the form allows the requesting physician to indicate that an expedited review is necessary. This option should be supported by appropriate documentation detailing the urgency of the employee’s condition.
- Detailed Request Information: The form requires specific details about the requested treatment, including the diagnosis, ICD code, and the service or good requested, along with the applicable CPT/HCPCS code, if known. Additional information such as frequency, duration, and quantity may also be necessary, depending on the nature of the request.
- Signature Requirements: The requesting physician’s signature is mandatory on the DWC Form RFA. This attestation confirms the necessity and validity of the request for the specified medical treatment, ensuring that the form is correctly processed by the claims administrator or Utilization Review Organization (URO).
- Claims Administrator/URO Response: Upon receipt, the claims administrator must respond to the request within the mandated timeframes, as outlined in the Labor Code and relevant California regulations. Their response can approve, deny, or modify the request and must be communicated back to the requesting provider, potentially using the same form for efficiency and clarity.
These takeaways highlight the importance of accuracy, detail, and adherence to regulatory requirements when completing the DWC Form RFA. Correctly filling out and submitting this form is a critical step in ensuring that employees receive the medical treatment they need for injuries or illnesses sustained while on the job. Additionally, understanding the response process by claims administrators or UROs is crucial for providers to navigate subsequent steps, including any necessary appeals or resubmissions.
Discover More PDFs
Judicial Council Form - Approved by the California Judicial Council, affirming its official status and reliability for court submissions.
What Is a Dmv Sr1 Form - Helps in providing a comprehensive account of the accident, including information about all parties and vehicles involved.
California Tax Efile - Withholding from California sources, estimated payments, and other credits are reconciled to determine the final tax obligation or refund.