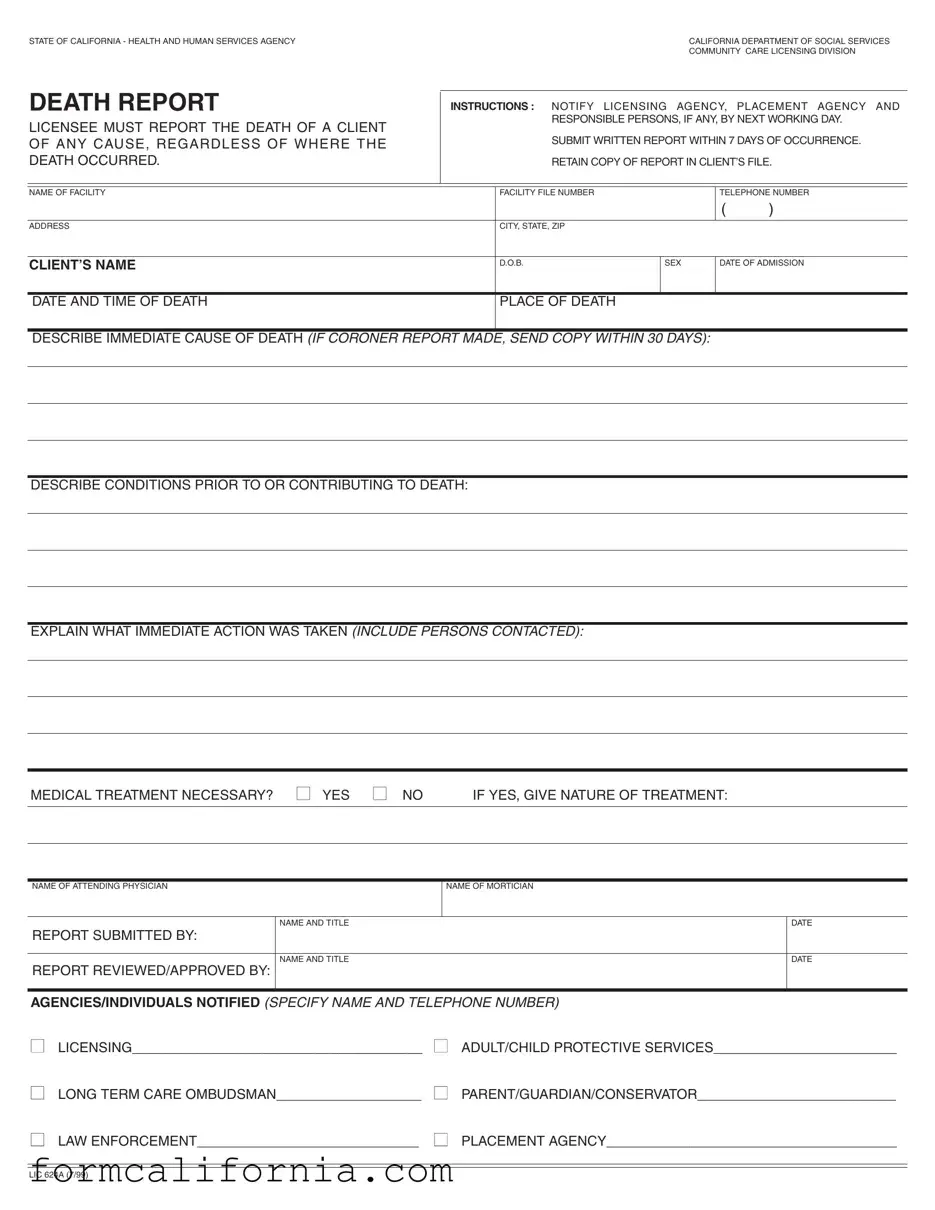
Blank Ca Death Report PDF Form
When it comes to the regulation and oversight of healthcare and social services within the State of California, detailed and timely documentation is a cornerstone of ensuring accountability and quality of care. Among the various reports that facilities are required to submit, the California Death Report form plays a critical role. This form, officially known as LIC 624A and issued by the California Department of Social Services Community Care Licensing Division, mandates that licensed facilities report the death of a client to several key agencies by the next working day following the event. Additionally, a written report must be submitted within seven days of the occurrence, covering aspects such as the client’s personal details, the time and place of death, a description of the immediate cause of death, and any contributing conditions. It’s also imperative for the facility to detail any immediate actions taken post-incident, specify if medical treatment was necessary, and list the personnel involved, including the attending physician and mortician. Keeping a copy of the report in the client’s file is not just a procedural requirement; it serves as a record for the facility and aids in maintaining transparency with regulatory bodies and the client's family or responsible parties. Through this, the form not only ensures that the relevant authorities and individuals are notified in a timely manner but also fosters a system of checks and balances within the care provision sector.
Document Preview Example
STATE OF CALIFORNIA - HEALTH AND HUMAN SERVICES AGENCY |
CALIFORNIA DEPARTMENT OF SOCIAL SERVICES |
|
COMMUNITY CARE LICENSING DIVISION |
DEATH REPORT |
INSTRUCTIONS : NOTIFY LICENSING AGENCY, PLACEMENT AGENCY AND |
||||||
LICENSEE MUST REPORT THE DEATH OF A CLIENT |
|
RESPONSIBLE PERSONS, IF ANY, BY NEXT WORKING DAY. |
|||||
|
|
|
|
|
|
||
OF ANY CAUSE, REGARDLESS OF WHERE THE |
|
SUBMIT WRITTEN REPORT WITHIN 7 DAYS OF OCCURRENCE. |
|||||
DEATH OCCURRED. |
|
RETAIN COPY OF REPORT IN CLIENT’S FILE. |
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
NAME OF FACILITY |
|
FACILITY FILE NUMBER |
|
TELEPHONE NUMBER |
|||
|
|
|
|
|
( |
) |
|
|
|
|
|
|
|
|
|
ADDRESS |
|
CITY, STATE, ZIP |
|
|
|
|
|
|
|
|
|
|
|
|
|
CLIENT’S NAME |
|
D.O.B. |
SEX |
DATE OF ADMISSION |
|||
|
|
|
|
|
|
|
|
DATE AND TIME OF DEATH |
|
PLACE OF DEATH |
|
|
|
|
|
|
|
|
|
|
|
|
|
DESCRIBE IMMEDIATE CAUSE OF DEATH (IF CORONER REPORT MADE, SEND COPY WITHIN 30 DAYS): |
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
DESCRIBE CONDITIONS PRIOR TO OR CONTRIBUTING TO DEATH: |
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
EXPLAIN WHAT IMMEDIATE ACTION WAS TAKEN (INCLUDE PERSONS CONTACTED): |
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
MEDICAL TREATMENT NECESSARY? ■ YES ■ NO |
IF YES, GIVE NATURE OF TREATMENT: |
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
NAME OF ATTENDING PHYSICIAN |
NAME OF MORTICIAN |
|
|
|
|
||
|
|
|
|
|
|
|
|
|
NAME AND TITLE |
|
|
|
|
|
DATE |
REPORT SUBMITTED BY: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
NAME AND TITLE |
|
|
|
|
|
DATE |
REPORT REVIEWED/APPROVED BY: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
AGENCIES/INDIVIDUALS NOTIFIED (SPECIFY NAME AND TELEPHONE NUMBER)
■LICENSING______________________________________ ■ ADULT/CHILD PROTECTIVE SERVICES________________________
■LONG TERM CARE OMBUDSMAN___________________ ■ PARENT/GUARDIAN/CONSERVATOR__________________________
■LAW ENFORCEMENT_____________________________ ■ PLACEMENT AGENCY______________________________________
LIC 624A (7/99)
Document Specs
| Fact | Detail |
|---|---|
| Form Title | Death Report |
| Agency | California Department of Social Services Community Care Licensing Division |
| Primary Purpose | To report the death of a client to relevant authorities and parties by the next working day and submit a written report within 7 days. |
| Governing Law | California Health and Human Services Agency regulations |
| Documentation Required | A copy of the coroner report must be sent within 30 days if a coroner report is made. |
| Notification Requirements | Licensing Agency, Placement Agency, Licensee, Protective Services, Long Term Care Ombudsman, Parent/Guardian/Conservator, and Law Enforcement must be notified. |
| Client Information | Includes name, date of birth, sex, date of admission, date and time of death, and the place of death. |
| Additional Information | Facilities must describe the immediate cause of death, conditions contributing to death, and any immediate actions taken, including medical treatment and individuals contacted. |
Detailed Instructions for Writing Ca Death Report
After a death occurs within a California Community Care Licensing Division facility, it's crucial to handle the reporting process correctly and promptly. This not only ensures compliance with state regulations but also helps in maintaining a transparent and responsible care environment. The California Death Report form, known as LIC 624A, is designed to gather all necessary information related to a client's death, ensuring that it is accurately reported to relevant agencies and individuals. The steps outlined below will guide you through completing this form thoroughly and efficiently.
- Start by entering the Name of Facility, Facility File Number, and the facility's Telephone Number at the top of the form.
- Provide the facility's Address, including City, State, and Zip.
- Fill in the Client’s Name, Date of Birth (D.O.B.), and Sex.
- Enter the Date of Admission to the facility and the Date and Time of Death.
- Specify the Place of Death.
- Describe the Immediate Cause of Death. If a coroner's report was made, remember to send a copy within 30 days.
- Detail any Conditions Prior to or Contributing to Death.
- Explain what Immediate Action Was Taken following the death, including persons contacted.
- Indicate whether Medical Treatment was necessary before death by checking Yes or No. If yes, provide the nature of the treatment.
- Record the Name of Attending Physician and the Name of Mortician.
- Fill in the Name and Title of the person submitting the report, and the date it was submitted.
- Note the Name and Title of the person who reviewed and approved the report, along with the approval date.
- List all Agencies/Individuals Notified about the death, including their names and telephone numbers. Specific agencies to notify include Licensing, Adult/Child Protective Services, Long Term Care Ombudsman, Parent/Guardian/Conservator, Law Enforcement, and Placement Agency.
Once completed, ensure that this form is submitted to the licensing agency, placement agency, and any responsible persons by the next working day following the death. A written report must be completed within seven days of the death occurring. Additionally, retain a copy of this report in the client’s file for future reference. Completing this form accurately and in a timely manner is crucial for compliance and for keeping all necessary parties informed.
Things to Know About This Form
What is the purpose of the California Death Report form?
The California Death Report form serves an important role in the state's health and human services infrastructure. It is used to document and report the death of a client to the necessary authorities, ensuring that all relevant parties are informed. This includes the California Department of Social Services, the Community Care Licensing Division, and other specified agencies. The form helps in maintaining transparency and accountability within facilities caring for individuals, and aids in ensuring compliance with state regulations regarding the reporting of deaths.
Who must complete and submit the California Death Report form?
The responsibility to complete and submit the California Death Report form falls on the facility where the client was receiving care. This includes notifying the licensing agency, placement agency, and any responsible persons associated with the client by the next working day following the client's death. A written report must then be submitted within seven days of the occurrence. This ensures that all relevant parties are promptly informed about the event and can take necessary actions in accordance with regulations and the individual's care plans.
What information is required on the California Death Report form?
The form requires detailed information about both the facility and the client. Key pieces of information include:
- The name, file number, telephone number, and address of the facility.
- The client's name, date of birth, sex, date of admission to the facility, date and time of death, and place of death.
- A description of the immediate cause of death and, if available, a copy of the coroner's report.
- Details regarding any conditions prior to or contributing to the death.
- An explanation of the immediate action taken following the death, including the names of persons contacted.
- Information concerning whether medical treatment was necessary and the nature of any treatment provided.
- The name of the attending physician and mortician, if applicable.
Additionally, the form requires the names, titles, and signatures of those submitting and reviewing the report, along with a section to list the agencies and individuals that were notified.
What actions should be taken immediately after a death occurs in a facility?
Upon the occurrence of a death in a facility, it is essential to promptly take the following actions:
- Contact and notify local licensing agencies, placement agencies, and responsible individuals about the death by the next working day.
- Prepare a detailed written death report, to be submitted within seven days of the death.
- Take immediate care actions as necessary, which may include contacting medical professionals, the coroner's office, or arranging mortuary services.
- Retain a copy of the death report in the client's file for record-keeping purposes.
These steps ensure that the situation is handled respectfully and in compliance with legal requirements.
Is a coroner's report always required to be submitted with the California Death Report form?
A coroner's report is to be submitted with the California Death Report form if such a report is made. This would usually happen in cases where the death was unexpected or the cause of death is not immediately clear. Including the coroner's report, if available, within 30 days of occurrence provides vital information for the proper documentation of the death and assists in the investigation and understanding of the circumstances surrounding the death.
Who should be notified of the death according to the California Death Report form?
According to the instructions on the California Death Report form, several entities and individuals must be notified in the event of a client's death. These include:
- The licensing agency overseeing the facility.
- The placement agency responsible for the client's care placement.
- Any responsible persons related to the client, such as a parent, guardian, or conservator.
- Adult or Child Protective Services, if applicable.
- The Long Term Care Ombudsman program.
- Law enforcement, when necessary.
Notifying these parties ensures that the death is properly recorded and that any follow-up actions, such as investigations or support for the family, can be initiated in a timely fashion.
Common mistakes
Filling out the California Death Report form requires attention to detail and a clear understanding of the instructions provided. People often make mistakes during this crucial process, which can lead to delays or inaccuracies in the reporting. Here are ten common mistakes made when completing the form:
Delay in notification: One of the first steps involves notifying the licensing agency, placement agency, and responsible persons by the next working day. Failure to promptly notify these entities is a common oversight.
Incomplete information: Not thoroughly filling out every section of the form is a frequent issue. Each detail, from the client’s name to the facility file number, plays a vital role in the report.
Forgetting to include the time of death alongside the date can compromise the accuracy of the report. Precise timing can be crucial for understanding the circumstances leading to death.
Omitting the immediate cause of death or providing a vague description hampers the accuracy of the report. If a coroner’s report is made, failing to send a copy within 30 days is also a mistake often made.
Sometimes, the conditions prior to or contributing to death are either left blank or not described in enough detail, which can obscure potential issues within the facility that need to be addressed.
Not specifying what immediate action was taken following the death, including the persons contacted, lacks critical information that could impact investigations or future care practices.
A common error is incorrectly answering or overlooking the query about medical treatment being necessary. If medical treatment was necessary, it's essential to detail the nature of the treatment.
The names and contact details of the attending physician and mortician are sometimes inaccurately provided or entirely missed, hindering further communication.
Agencies and individuals notified section often suffers from incomplete entries. It’s critical to specify each contacted entity’s name and telephone number for records and follow-up.
Finally, ensuring that the form is submitted and reviewed by the required dates is a step frequently overlooked. The date report submitted by and the date report reviewed/approved by sections must not be ignored.
Steering clear of these mistakes can significantly enhance the quality of reporting and ensure that all necessary parties are properly informed. This can facilitate a smoother process for all involved and contribute to the ongoing effort of providing quality care and accountability within California's healthcare facilities.
Documents used along the form
When dealing with the complexities surrounding the end of a life, the California Death Report Form stands as a crucial document. However, navigating the aftermath of a death involves more than filling out this single form. Various other forms and documents often come into play, each serving its unique role in the procedural tapestry designed to ensure all aspects of a person’s passing are handled with dignity and in accordance with legal requirements.
- Certificate of Death (VS-112 Form): This official document certifies the death of an individual. It is a vital record that provides crucial information such as the cause of death, date, and place. This certificate is necessary for legal purposes, including estate settlement and benefits claims.
- Coroner's Report: A Coroner's Report provides detailed findings from an autopsy if conducted, including the cause of death, especially in cases where the death was sudden, unexpected, or the result of unusual circumstances. This report can be essential for both legal and medical reasons, helping to clarify the events leading to the death.
- Notice of Death to Social Security Administration: This document notifies the Social Security Administration of a death, ensuring that benefits are properly adjusted and preventing fraud. The notification process is crucial for the timely update of records and management of survivor benefits, if applicable.
- Authorization for Cremation and Disposition (Cremation Permit): In cases where cremation is chosen, this authorization form is required. It grants permission for the body to be cremated and outlines the final disposition of the ashes, ensuring that the process respects the wishes of the deceased and their family.
These documents, alongside the California Death Report Form, form a network of paperwork that guides those dealing with loss through the necessary legal steps. Each document carries its own weight, ensuring that every aspect of a person’s passing is accounted for with sensitivity and compliance. Understanding and utilizing these forms helps to ease the bureaucratic burden on grieving families, allowing them to focus more on remembering their loved ones and less on navigating governmental red tape.
Similar forms
The California Death Report form shares similarities with a Birth Certificate. Both documents serve as official records maintained by state agencies, documenting critical life events. Like the Death Report, a Birth Certificate includes personal identifiers (name, sex, date of birth), relevant dates (of birth for Birth Certificates and of death for the Death Report), and data regarding the location of the event (place of birth/death). However, while a Death Report focuses on the end of life, including causes and conditions leading to death, a Birth Certificate records the commencement of life, capturing details pertinent to the birth.
Comparable to an Autopsy Report, the California Death Report form encompasses details about a person’s death, including the time, place, and immediate causes. An Autopsy Report delves deeper into the cause of death through examination, providing insights that might not be immediately apparent, similar to the Death Report's section on conditions contributing to death. Both documents play a vital part in health statistics and legal matters, helping to clarify circumstances surrounding a death.
Similar to an Incident Report filed in healthcare facilities, the California Death Report form includes documentation of an event (in this case, a death) and the immediate actions taken in response. Like Incident Reports, which detail accidents or unexpected events within a facility, the Death Report requires information on how the situation was handled, including medical treatment and notification of responsible parties. Both forms are crucial for compliance and risk management within care settings.
An Advance Directive is another document that, like the California Death N/Aeport form, deals with the circumstances surrounding an individual’s health and end-of-life decisions. While an Advance Directive outlines a person’s preferences for treatment and care in anticipation of incapacitation, the Death Report documents what occurred at life’s end, including treatments administered. Each serves to ensure that an individual’s health care preferences are respected, albeit at different stages of care.
The Patient's Medical Record, which chronicles an individual's medical history, treatments received, and outcomes, bears resemblance to the sections of the California Death Report form detailing medical conditions and treatments prior to death. Both documents are fundamental to understanding the health trajectory leading to the patient's current status or, in the case of the Death Report, the cause of death. This similarity highlights their roles in ensuring continuity and quality of care.
Police Reports, like the California Death Report form, document specific events - in the former's case, crimes or incidents involving law enforcement. Both forms include factual accounts of what happened, individuals involved, and actions taken immediately following the event. While Police Reports may cover a wide range of incidents, the Death Report is specifically focused on the details and circumstances of an individual’s death, including any law enforcement notification.
The Obituary, a publicly shared announcement of someone's death, shares a common purpose with the California Death Report form in notifying relevant parties about a death. While an Obituary typically includes a brief biography, surviving family members, and funeral arrangements, the Death Report provides detailed official records of the death, including medical and administrative details. Both serve to inform and document, but from different perspectives and for varied audiences.
Dos and Don'ts
Completing the California Death Report form requires careful attention to detail and adherence to specific protocols to ensure accuracy and compliance. Below are essential dos and don'ts to consider during the process.
Things You Should Do
- Immediately notify the licensing agency, placement agency, and responsible persons, if any, about the death of a client by the next working day, ensuring timely communication.
- Accurately fill in all sections of the form, including the facility's information, client details, and specifics about the death, to provide a comprehensive report.
- Include detailed descriptions of the immediate cause of death and any conditions prior to or contributing to death, which may require gathering precise information from medical personnel or records.
- Attach a copy of the coroner's report if one was made, submitting it within 30 days to provide official documentation of the death.
- Retain a copy of the completed report in the client's file for future reference and compliance with record-keeping requirements.
Things You Shouldn't Do
- Avoid delays in the notification of the death to all required agencies and individuals, as failing to do so by the next working day can lead to non-compliance issues.
- Do not leave sections of the form blank or provide incomplete information, as this can result in the need for follow-up and potential delays in the processing of the death report.
- Refrain from submitting the form without a thorough review, which may lead to errors or omissions in the reported information.
- Avoid guessing details when uncertain, especially regarding the cause of death or medical conditions. Instead, consult with medical professionals or look at medical records to ensure accuracy.
- Do not neglect to notify all listed agencies and individuals, including licensing, adult/child protective services, the long-term care ombudsman, and any law enforcement or placement agencies involved, as each has a role in the subsequent processes after a death occurs.
Misconceptions
There are several misconceptions about the California Death Report form commonly held by individuals who may need to interact with or complete the form. It's important to address these misconceptions to ensure the form is correctly understood and used.
Only deaths that occur within the facility need to be reported: Contrary to this belief, the death of a client must be reported regardless of where it occurs. This includes deaths that happen while the client is outside the facility.
A verbal notification is sufficient: While immediate notification to the licensing agency, placement agency, and responsible persons is crucial, a written report must also be submitted within 7 days of the death. Merely informing the relevant parties verbally does not fulfill the reporting requirements.
The report is optional if the cause of death is natural: There is a misconception that if a client dies of natural causes, reporting is not necessary. However, all deaths, regardless of the cause, must be reported. The form explicitly requires the cause of death to be described, including conditions contributing to the death.
Keeping a copy of the report is unnecessary: Facilities might believe once they’ve submitted the report to the appropriate agencies, there's no need to retain a copy. The instructions clearly state that a copy of the report must be kept in the client's file, emphasizing the importance of record-keeping.
Only the licensing agency needs to be notified: The instructions necessitate notifying not just the licensing agency but also the placement agency, and where applicable, responsible persons. Depending on circumstances, adult/child protective services, the Long Term Care Ombudsman, law enforcement, and the parent/guardian/conservator may also need to be informed.
Details about immediate actions taken are not crucial: Every detail regarding immediate actions taken following the client's death is vital. This includes persons contacted and measures undertaken before the report was filed. This information is critical for transparency and accountability.
If a coroner's report is made, submitting the death report isn't urgent: Despite the involvement of a coroner, the facility is still required to submit the death report within 7 days. If a coroner's report is made, a copy should be sent to the licensing agency within 30 days, but this does not negate the need for timely submission of the death report.
Addressing these misconceptions ensures that the death report form is accurately completed and submitted in compliance with the requirements of the California Department of Social Services Community Care Licensing Division, thereby upholding the facility's legal obligations and ensuring the well-being and rights of clients are respected even in death.
Key takeaways
When dealing with the tragic event of a client's death, those responsible within California's healthcare facilities must navigate the process with sensitivity and adherence to specific regulations. The California Death Report form, required by the California Department of Social Services, is a crucial document in this process. Here are nine key takeaways about filling out and using the California Death Report form:
- Timely Notification is Crucial: The death of a client must be reported to the licensing agency, placement agency, and responsible persons, if any, by the next working day following the death. This quick turnaround ensures all necessary parties are informed promptly.
- Submission Deadline: A written report detailing the death must be submitted within seven days of its occurrence. This report should provide a comprehensive account of the event and any relevant circumstances.
- Record Retention: A copy of the death report must be retained in the client’s file. This helps maintain a complete record of the client’s history within the facility.
- Comprehensive Information Required: The form requires detailed information, including the client’s name, date of birth, sex, date of admission to the facility, the date and time of death, and the place of death. Providing complete information is essential for a thorough documentation process.
- Cause of Death: The immediate cause of death must be described on the form. If a coroner's report is made, a copy of it must be sent within 30 days. This helps in understanding the circumstances leading to the death.
- Conditions and Actions: The form asks for descriptions of the conditions contributing to the death and the immediate actions taken following the death. This section highlights the facility’s response and any medical treatment provided.
- Medical Treatment: It’s required to specify whether medical treatment was necessary, and if so, the nature of the treatment. This information contributes to a fuller picture of the client’s final days and the care they received.
- Notification Record: The form requires a list of all agencies and individuals notified about the death. This includes licensing agencies, protective services, law enforcement, and the client’s parent, guardian, or conservator. Documenting these notifications ensures accountability and compliance with reporting obligations.
- Review and Approval: The names and titles of the individuals who submitted and reviewed or approved the report are necessary. This ensures that the report is meticulously checked for accuracy and completeness.
Properly filling out and handling the California Death Report form is a responsibility that facilities must take seriously. It not only complies with state regulations but also ensures dignity and respect for the deceased and their families during a difficult time.
Discover More PDFs
California 501c3 - An express address to mail the request facilitates a clear directive for submission, ensuring documents reach the right department.
Osha 5020 - It includes sections for employers to fill out regarding the employee’s personal information, job title, and the date and time of the injury or incident.